PCOS vs Cushing's: When to Suspect Each Condition
Explore the differences between PCOS and Cushing's Syndrome, including symptoms, diagnosis, and management for better health outcomes.
Explore the differences between PCOS and Cushing's Syndrome, including symptoms, diagnosis, and management for better health outcomes.
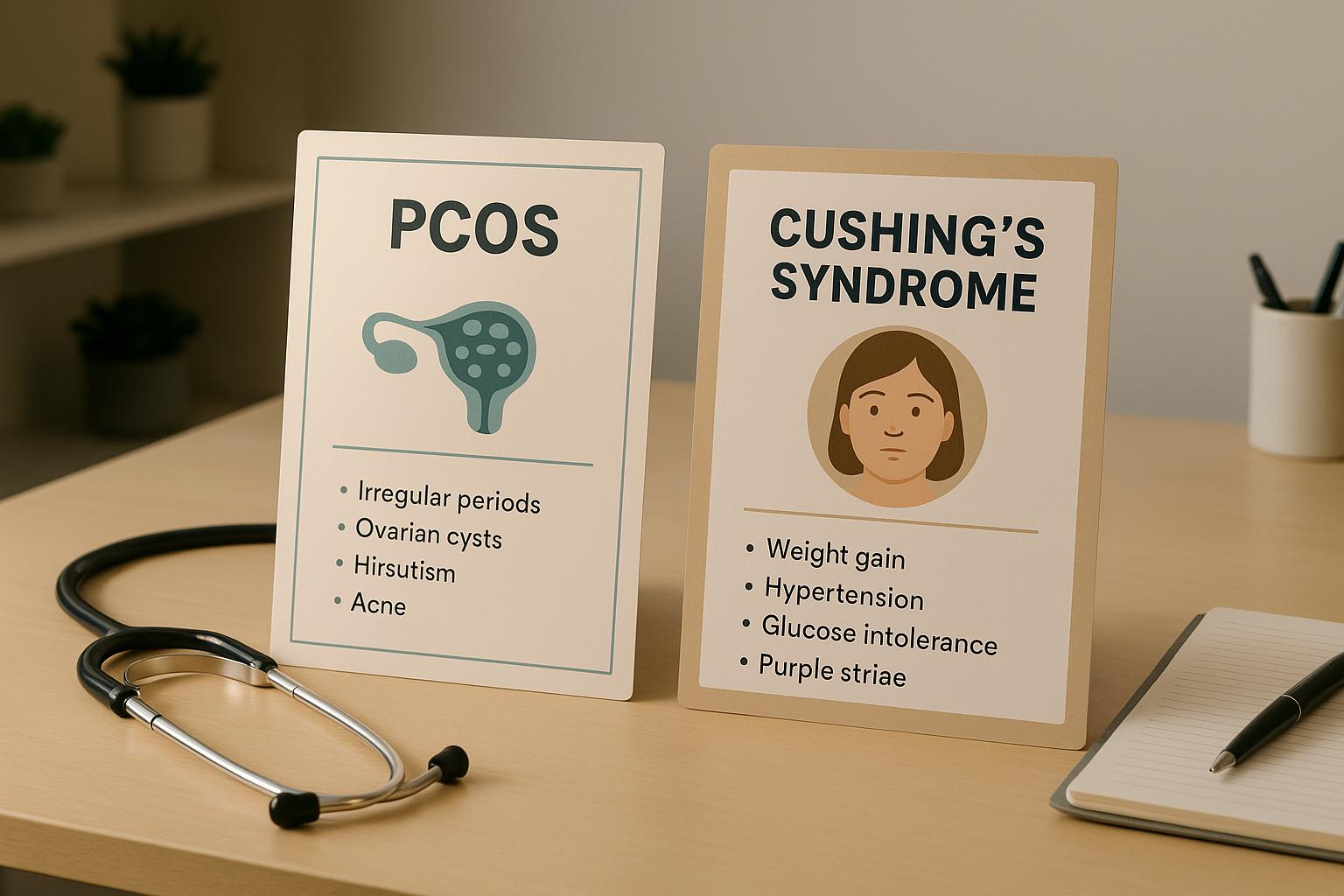
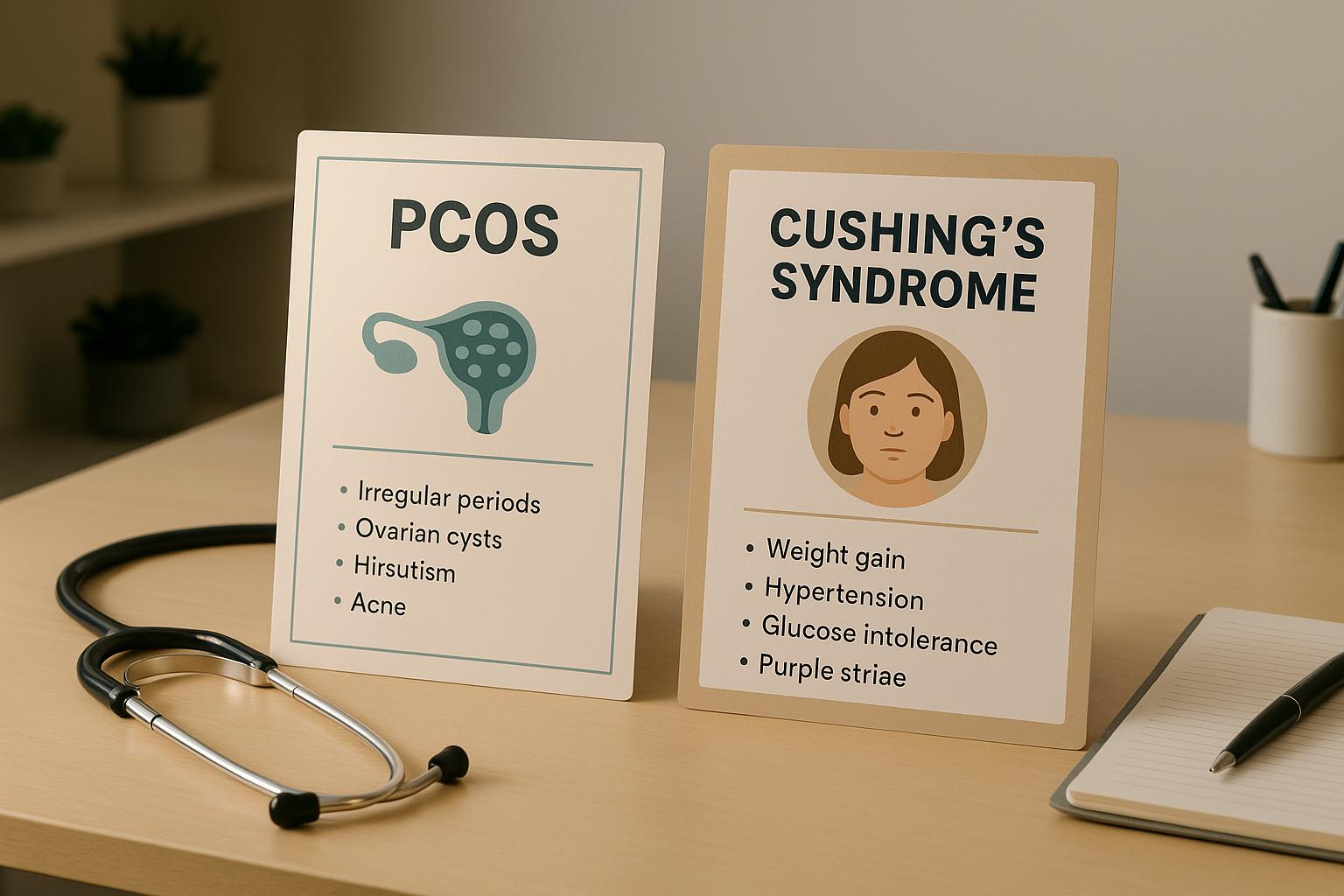
If you're dealing with weight gain, irregular periods, or excess hair growth, it could be PCOS or Cushing's Syndrome. While these conditions share symptoms, they have distinct causes and treatments. PCOS is tied to insulin resistance and high androgen levels, affecting 1 in 10 women of reproductive age. Cushing's, caused by excess cortisol, is much rarer, impacting 10–15 people per million annually. Here's how to tell them apart:
Diagnosis:
Quick Comparison:
| Feature | PCOS | Cushing's Syndrome |
|---|---|---|
| Cause | Insulin resistance, androgens | Excess cortisol |
| Key Symptoms | Polycystic ovaries, dark patches | Moon face, buffalo hump |
| Tests | Hormone/metabolic tests | Cortisol and imaging tests |
| Prevalence | ~10% of women (reproductive age) | 10–15 cases per million/year |
If you're noticing these signs, consult a doctor. Early diagnosis is critical for managing PCOS or addressing Cushing's, which often requires urgent care.
Understanding the symptom patterns of PCOS and Cushing's Syndrome can help pinpoint the right diagnosis. While these conditions share several overlapping symptoms, each has unique traits that can offer crucial diagnostic clues.
Both PCOS and Cushing's Syndrome often lead to weight gain, particularly around the midsection. This shift in fat distribution can make your clothes feel tighter at the waist, as both conditions affect how your body stores fat.
Another common symptom is irregular menstrual cycles. This might mean periods that are too frequent, too infrequent, or even absent for months. Some women may also experience unpredictable bleeding patterns.
Hirsutism, or excessive hair growth in typically male areas, is another shared feature. This includes coarse, dark hair appearing on the face, chest, back, or abdomen. Over time, this hair growth often becomes more noticeable.
Persistent acne is also a hallmark of both conditions. This type of acne, often resistant to over-the-counter treatments, tends to appear on the face, chest, and back.
Mood changes like depression, anxiety, and irritability are frequently reported. These emotional shifts can disrupt relationships and daily life.
Finally, both conditions can lead to fertility challenges. While the underlying reasons differ, both PCOS and Cushing's Syndrome can interfere with ovulation, making it harder to conceive.
Now, let’s take a closer look at symptoms unique to each condition.
PCOS has several hallmarks that set it apart. One of the most recognizable is polycystic ovaries, which can be seen on an ultrasound. These ovaries often display a "string of pearls" appearance due to multiple small cysts lining their edges, though not all women with PCOS will have this feature.
Insulin resistance is another key trait, affecting up to 70% of women with PCOS. This can lead to intense sugar cravings, energy crashes after meals, and difficulty managing weight.
Dark, velvety skin patches, known as acanthosis nigricans, often appear in areas like the neck, armpits, or groin. These patches are linked to insulin resistance and are rarely seen in Cushing's Syndrome.
Male-pattern baldness, such as thinning hair at the temples or crown, is another symptom specific to PCOS.
While PCOS has its own set of distinct signs, Cushing's Syndrome presents a different range of unique features.
Cushing's Syndrome causes several physical changes that don’t occur with PCOS. One of the most noticeable is moon face, a round, full appearance of the face caused by fat redistribution. Family members are often the first to point this out.
Another hallmark is the buffalo hump, a fatty deposit that forms between the shoulder blades at the base of the neck, creating a hump-like appearance.
Purple stretch marks (striae) are a key indicator. Unlike the pink or white stretch marks seen with weight changes, these marks are deep purple or reddish and often wider. They typically appear on the abdomen, thighs, arms, and breasts.
Easy bruising and slow wound healing are common due to the impact of excess cortisol on blood vessels and the body's repair mechanisms. You might notice bruises from minor bumps or cuts taking much longer to heal.
Muscle weakness, particularly in the arms and legs, can make daily activities like climbing stairs or lifting objects more difficult.
High blood pressure and high blood sugar tend to develop more severely and quickly in Cushing's Syndrome, often requiring immediate medical attention.
Lastly, cognitive changes such as memory issues, trouble focusing, and mood swings are more pronounced with Cushing's Syndrome. Many describe it as feeling like they're in a mental fog, which can affect work and personal life.
Here’s a quick breakdown of the differences:
| PCOS Only | Shared Symptoms | Cushing's Syndrome Only |
|---|---|---|
| Polycystic ovaries on ultrasound | Weight gain (especially abdominal) | Moon face |
| Insulin resistance symptoms | Irregular menstrual cycles | Buffalo hump |
| Acanthosis nigricans (dark skin patches) | Hirsutism (excess hair growth) | Purple stretch marks |
| Male-pattern hair loss | Adult acne | Easy bruising |
| Intense sugar cravings | Mood changes (depression, anxiety) | Muscle weakness |
| Energy crashes after meals | Fertility difficulties | Severe high blood pressure |
| Rapid cognitive changes | ||
| Slow wound healing |
Recognizing these distinctions is essential for guiding diagnostic tests and treatment plans. While shared symptoms can make the initial diagnosis tricky, the unique traits of each condition can help your healthcare provider decide which tests to prioritize and what to focus on during your evaluation.
PCOS and Cushing's Syndrome stem from different hormonal imbalances that impact the body in unique ways. These differences are key to understanding why their treatments vary so widely.
PCOS disrupts your body's systems by increasing androgens - hormones like testosterone typically associated with male characteristics. This excess of androgens causes the ovaries to malfunction, leading to multiple cysts and irregular or absent egg release.
A major driver of this imbalance is insulin resistance. When your cells don't respond effectively to insulin, the pancreas compensates by producing more. This extra insulin signals the ovaries to ramp up androgen production. About 70% of women with PCOS have insulin resistance, creating a vicious cycle where high insulin levels worsen hormonal issues.
Another key factor is consistently elevated luteinizing hormone (LH). Normally, LH surges once a month to trigger ovulation, but in PCOS, it stays high, fueling more androgen production and preventing normal egg release.
These hormonal shifts are what lead to the hallmark symptoms of PCOS, including male-pattern hair growth, metabolic challenges, and fertility problems.
Cushing's Syndrome, on the other hand, results from prolonged exposure to high levels of cortisol, the body's primary stress hormone. This chronic cortisol excess disrupts multiple systems in the body.
The condition typically arises from one of three sources. Pituitary adenomas - benign tumors in the pituitary gland - cause about 80% of cases by overproducing ACTH (adrenocorticotropic hormone), which signals the adrenal glands to release too much cortisol. Other causes include adrenal tumors, which directly produce cortisol, and ectopic ACTH syndrome, where tumors in other parts of the body inappropriately produce ACTH.
Excess cortisol has widespread effects: it breaks down muscle, redistributes fat to areas like the face and upper back, weakens the immune system, elevates blood pressure and blood sugar, and even disrupts sleep and cognitive function. These effects make Cushing's Syndrome a complex condition requiring targeted diagnostic and treatment strategies.
The groups most affected by these conditions highlight their distinct hormonal roots.
PCOS primarily affects women of reproductive age, with symptoms often starting during or after puberty. It impacts 6% to 12% of women in the U.S. during their childbearing years. Genetics play a significant role - having a mother or sister with PCOS increases the risk. Additionally, higher rates are observed among Hispanic, African American, and Middle Eastern women.
Cushing's Syndrome, however, affects a broader demographic, most commonly adults aged 25 to 40. While both men and women can develop the condition, women are diagnosed three times more often. It’s also far rarer than PCOS, affecting only 10 to 15 people per million each year. Because it’s caused by tumors or structural abnormalities rather than metabolic factors, geographic or lifestyle influences don’t play a role. That said, long-term use of corticosteroids can mimic Cushing's symptoms.
These demographic differences explain why PCOS screenings focus on reproductive-age women with metabolic symptoms, while Cushing's evaluations consider a wider range of individuals showing systemic issues.
Getting the right diagnosis can bring clarity after years of unexplained symptoms. The processes for diagnosing PCOS and Cushing's Syndrome differ significantly because they involve entirely different hormonal systems.
Diagnosing PCOS starts with identifying a pattern of symptoms. Doctors often use the Rotterdam criteria, which require meeting two out of three conditions: irregular or absent menstrual cycles, signs of high androgen levels, and polycystic ovaries visible on an ultrasound.
Blood tests are essential for diagnosing PCOS. Total and free testosterone levels are measured, as elevated levels signal androgen excess. The androstenedione test is another tool to confirm increased androgen production. Additionally, doctors may check DHEA-S (dehydroepiandrosterone sulfate) to rule out other causes of high androgen levels.
Since insulin resistance plays a major role in PCOS, metabolic testing is also critical. A fasting glucose test and a 2-hour glucose tolerance test can reveal pre-diabetes or diabetes. Although not always covered by insurance, a fasting insulin test provides valuable insights into the severity of insulin resistance.
A pelvic ultrasound examines the ovaries for the "string of pearls" appearance - multiple small follicles that are characteristic of PCOS. However, ultrasound findings are considered alongside other symptoms for a diagnosis.
Exclusion tests help rule out other conditions with similar symptoms. For example, thyroid function tests (TSH and free T4) can identify thyroid disorders, prolactin levels screen for pituitary issues, and the 17-hydroxyprogesterone test checks for congenital adrenal hyperplasia, a genetic condition that can mimic PCOS.
While PCOS diagnosis relies on hormonal and metabolic patterns, Cushing's Syndrome requires a different approach - proving cortisol excess.
Diagnosing Cushing's Syndrome involves confirming excessive cortisol production and identifying its source. Because cortisol levels naturally fluctuate and are influenced by stress, illness, and medications, multiple rounds of testing are often required.
Initial screening tests measure cortisol levels over an extended period. The 24-hour urine cortisol test evaluates daily cortisol production, with normal levels typically below 50–100 micrograms per 24 hours, depending on the lab. The late-night salivary cortisol test takes advantage of cortisol's natural rhythm - levels should drop significantly by 11 PM, but they remain elevated in Cushing's Syndrome.
Another common test is the overnight dexamethasone suppression test, where you take 1 mg of dexamethasone (a synthetic steroid) at 11 PM and have blood drawn at 8 AM the next morning. In healthy individuals, dexamethasone suppresses cortisol production to below 1.8 micrograms per deciliter. Higher levels suggest Cushing's Syndrome.
Once cortisol excess is confirmed, the next step is source identification. The high-dose dexamethasone suppression test can help distinguish between pituitary and non-pituitary causes. Measuring ACTH levels provides additional clues: low ACTH suggests adrenal tumors, while high ACTH points to pituitary adenomas or ectopic ACTH syndrome.
Imaging studies are used to locate the source of the problem. MRI can detect pituitary adenomas as small as 3–4 mm, while CT scans of the adrenal glands can identify adrenal tumors or hyperplasia. If ectopic ACTH syndrome is suspected, whole-body imaging may be necessary to locate the source tumor.
Pinpointing the exact source of cortisol overproduction is essential for effective treatment.
| Aspect | PCOS Testing | Cushing's Syndrome Testing |
|---|---|---|
| Primary Focus | Androgen excess, ovarian dysfunction | Cortisol excess, source identification |
| Key Blood Tests | Total/free testosterone, androstenedione, fasting glucose, insulin | 24-hour urine cortisol, late-night salivary cortisol, ACTH |
| Specialized Tests | 2-hour glucose tolerance test, DHEA-S | Dexamethasone suppression tests (low and high dose) |
| Imaging | Pelvic ultrasound for ovarian structure | MRI (pituitary), CT (adrenal), possible whole-body imaging |
| Exclusion Tests | TSH, prolactin, 17-hydroxyprogesterone | Medication history review, stress assessment |
| Diagnostic Criteria | Rotterdam criteria (2 of 3 conditions) | Proven cortisol excess plus source identification |
| Testing Timeline | Usually completed in 1–2 visits | Often requires multiple rounds over weeks to months |
| Cost Considerations | Most tests covered by insurance | Extensive testing may require prior authorization |
The difference in diagnostic approaches reflects the unique nature of these conditions. PCOS diagnosis focuses on identifying a metabolic pattern, while Cushing's Syndrome requires confirming a specific biochemical imbalance and tracing its source. This explains why PCOS is often diagnosed relatively quickly, whereas Cushing's Syndrome can take much longer to confirm.
Now that you’re familiar with the symptoms and testing differences, it’s time to take action. Early steps can make a big difference for both PCOS and Cushing’s Syndrome.
If you’re noticing troubling symptoms, schedule an appointment with your primary care doctor right away. Keep a detailed record of your symptoms, noting when they occur, how severe they are, and any patterns you’ve noticed. For menstrual changes, tracking your cycle for a few months can provide helpful insights.
When meeting with your doctor, be as specific as possible about your concerns. For instance, instead of saying "I feel tired", explain that you’re sleeping 10 hours a night but still feel exhausted by the afternoon, or that you’re getting winded after climbing just a few stairs. These details can help your doctor better understand the severity of your symptoms and decide which tests to recommend.
If initial evaluations don’t fully address your concerns, don’t hesitate to push for further testing. Depending on your symptoms, your doctor may order specific tests to confirm or rule out PCOS or Cushing’s.
In some cases, it may be helpful to consult an endocrinologist. If hormonal imbalances are suspected, they can provide specialized care. For PCOS, a reproductive endocrinologist might be the right choice, especially if fertility is a concern.
Be prepared for multiple appointments. Diagnosing hormonal conditions can take time, particularly with Cushing’s Syndrome, which often requires months of testing to confirm. While the process can be lengthy, don’t hesitate to seek a second opinion if you feel your concerns aren’t being addressed.
Taking these steps early ensures you’re on the right path toward a proper diagnosis and effective treatment.
As discussed earlier, identifying the exact hormonal imbalance is key to determining the right treatment. PCOS and Cushing’s require very different approaches, so an accurate diagnosis is critical.
The long-term health risks of these conditions also differ. PCOS can increase the likelihood of type 2 diabetes, heart disease, and endometrial cancer, but these risks can often be managed with proper care. On the other hand, untreated Cushing’s Syndrome can lead to severe complications like bone fractures, serious infections, and life-threatening cardiovascular issues.
For those considering children, family planning challenges also vary. PCOS can affect fertility, but treatments like ovulation induction medications are often effective. Cushing’s Syndrome, however, can have a more significant impact on fertility and pregnancy outcomes, and treatment plans may need to be adjusted if you’re planning to conceive. A clear diagnosis ensures you receive the right guidance for your reproductive health.
Platforms like PCOSHelp offer valuable resources to support your care decisions. Their evidence-based guides cover everything from symptom management and treatment options to lifestyle adjustments like dietary changes for insulin resistance and stress management techniques. You’ll also find updates on the latest research, giving you tools to make informed choices about your care.
Getting the right diagnosis might take time, but it’s a crucial step toward feeling better. Both PCOS and Cushing’s Syndrome are treatable, and with the right approach, you can manage your condition effectively and improve your quality of life.
Telling the difference between PCOS and Cushing's Syndrome can be tricky since they share symptoms like weight gain, irregular periods, and mood swings. But understanding the distinct signs of each condition is key to getting the right care.
PCOS often comes with symptoms like excessive hair growth, acne, and challenges with fertility, which are tied to insulin resistance. On the other hand, Cushing's Syndrome is marked by features such as a rounded "moon face", deep purple stretch marks, and muscle weakness, all caused by too much cortisol. While PCOS primarily affects reproductive hormones and metabolism, Cushing's disrupts the body's stress hormone system.
Guesswork won’t cut it - diagnosing either condition requires specific medical tests. For PCOS, doctors look for irregular ovulation, high androgen levels, and polycystic ovaries visible on an ultrasound. Diagnosing Cushing's involves measuring cortisol levels through various tests, including suppression tests.
Timely action makes all the difference. Managing PCOS early can lower the chances of complications like type 2 diabetes and heart disease. Similarly, addressing Cushing's Syndrome quickly can help avoid serious issues like bone fractures and heart problems. Keep an eye on your symptoms, and don’t hesitate to consult your healthcare provider for thorough testing. Taking these steps can help you stay ahead of your health.
Distinguishing PCOS from Cushing's Syndrome can be tricky because they share overlapping symptoms, but there are key differences to look out for:
Although both conditions can cause symptoms like hirsutism and irregular periods, purple striae, muscle weakness, and a distinct facial appearance are more characteristic of Cushing's Syndrome. If you're uncertain about your symptoms, reaching out to a healthcare provider for testing and an accurate diagnosis is essential.
If you think you might have PCOS, talk to your doctor about these potential tests:
For Cushing's Syndrome, your doctor may recommend:
Make sure to share all your symptoms with your doctor so they can decide which tests are best for you. Identifying these conditions early can make a big difference in managing them effectively.
Managing PCOS often starts with lifestyle changes aimed at improving insulin sensitivity and balancing hormones. This includes focusing on a nutrient-rich, well-rounded diet, staying active with regular exercise, managing stress effectively, and ensuring you get enough quality sleep. These habits can help stabilize metabolism and alleviate symptoms like irregular menstrual cycles and weight gain.
For Cushing's Syndrome, the focus shifts to addressing the effects of elevated cortisol levels. Key strategies include eating a diet rich in protein and calcium, reducing salt intake to manage fluid retention, and incorporating gentle, low-impact exercises like walking or yoga. These activities help prevent overexertion and support bone strength.
While both conditions benefit from healthy eating and staying active, the goals differ. PCOS management prioritizes metabolic and hormonal balance, while Cushing's Syndrome care focuses on controlling cortisol levels and maintaining bone and muscle health.