PCOS Diagnosis: 3 Key Criteria Explained
Understand the key criteria for diagnosing PCOS, including symptoms, tests, and how it affects women's health.
Understand the key criteria for diagnosing PCOS, including symptoms, tests, and how it affects women's health.
PCOS (Polycystic Ovary Syndrome) affects up to 12% of women of reproductive age in the U.S., yet it often goes undiagnosed for years. Understanding the diagnostic process can help you take control of your health and discuss symptoms effectively with your doctor. Here’s a breakdown of the three main criteria used to diagnose PCOS, based on the widely accepted Rotterdam Criteria:
To officially diagnose PCOS, at least two of these criteria must be met. Doctors also rule out other conditions like thyroid disorders or congenital adrenal hyperplasia that can mimic PCOS symptoms. Early diagnosis and management are key to improving quality of life and reducing health risks like type 2 diabetes and heart disease.
High androgen levels play a central role in diagnosing PCOS. While androgens are naturally present in women, elevated levels can lead to symptoms that may disrupt daily life.
Healthcare providers evaluate hyperandrogenism by looking at two main factors: physical signs and blood test results.
When androgen levels are elevated, they often manifest through noticeable changes in hair growth and skin condition. One common sign is hirsutism, which refers to excessive hair growth in areas where men typically grow hair. This can include coarse, dark hair on the chin, upper lip, jawline, chest, back, or inner thighs.
Acne that persists or suddenly worsens - especially along the jawline, chin, and neck - may also point to androgen excess. Another potential sign is androgenic alopecia, a type of hair thinning often seen on the crown or temples. This can result in a visibly wider part or a thinner ponytail, which many women find distressing.
These physical changes are driven by elevated testosterone levels, prompting further medical evaluation.
Blood tests are essential to confirm high androgen levels. Key markers include total and free testosterone, with elevated levels of either supporting a diagnosis of hyperandrogenism in PCOS cases.
Additional tests for DHEA and DHEAS can also aid in diagnosis. While elevated levels of these hormones are consistent with PCOS, extremely high DHEAS levels might signal rare conditions like an androgen-secreting adrenal tumor.
Another important marker is Sex Hormone-Binding Globulin (SHBG). Low SHBG levels mean more active testosterone is circulating in the bloodstream, which is often associated with PCOS.
To rule out other conditions that might mimic PCOS symptoms, doctors also measure 17-hydroxyprogesterone (17-OHP). This test helps identify late-onset congenital adrenal hyperplasia, a condition that can present similarly. Hormone tests for thyroid-stimulating hormone (TSH), prolactin, FSH, and LH are also used to exclude other potential causes of symptoms.
Accurate testing is critical, but several factors can influence results. For example, the timing of the test within the menstrual cycle and certain medications can alter androgen levels. Birth control pills, in particular, can suppress androgen levels, potentially masking symptoms and leading to false-negative results. Your doctor may recommend stopping hormonal contraceptives before testing.
Supplements can also interfere with results. For instance, biotin, commonly found in multivitamins and hair or nail products, may skew some hormone test outcomes. Additionally, fasting requirements vary depending on the specific tests ordered, so it’s important to follow your healthcare provider’s instructions carefully.
It’s worth noting that the LH to FSH ratio, once considered a diagnostic marker for PCOS, is no longer widely used due to its variability depending on the menstrual cycle.
After assessing androgen levels, the next step in understanding PCOS's impact on fertility is to evaluate ovulation patterns. PCOS often interferes with ovulation, resulting in irregular or even absent menstrual cycles.
Unlike hormone-level evaluations alone, examining ovulation function gives a clearer picture of how PCOS affects the reproductive system. When ovulation becomes sporadic or halts entirely, the effects extend beyond missed periods, influencing overall fertility and hormonal balance.
In individuals with PCOS, the ovaries may rarely or never release eggs. This condition often manifests as oligomenorrhea (infrequent periods) or amenorrhea (no periods at all) [3-5]. While a typical menstrual cycle ranges from 21 to 35 days, PCOS can stretch cycles to over 40 days or even several months. These unpredictable patterns make it challenging to identify ovulation, directly impacting fertility. PCOS is responsible for infertility in up to 15% of women of reproductive age. Tracking these irregularities is a key part of diagnosis.
Keeping a detailed record of your menstrual history is essential. Note your cycle length, flow, and consistency over time. This information helps healthcare providers determine whether your cycles have always been irregular or if changes have occurred recently, which can help differentiate PCOS from other conditions. Using a calendar or a smartphone app to log this data is a practical approach. Providers may also ask about past pregnancies, birth control usage, and any medications that could influence your cycle.
Beyond tracking your cycles, hormone tests provide further insight into ovulation irregularities. Tests measuring hormones like luteinizing hormone (LH), follicle-stimulating hormone (FSH), and progesterone can clarify ovulation status. For example, progesterone levels naturally increase after ovulation, so consistently low levels during the second half of your cycle may indicate that ovulation hasn’t occurred. Additionally, a pelvic ultrasound can detect follicle cysts that form when ovulation is impaired. These cysts often appear in a "string of pearls" pattern along the ovary's edge, a hallmark of PCOS.
The third diagnostic criterion hones in on the physical characteristics of the ovaries. While the name "polycystic ovary syndrome" might suggest the presence of cysts, what doctors actually look for are multiple small follicles that create a specific pattern visible on ultrasound. These findings, when combined with hormonal and menstrual assessments, help form a complete diagnosis. However, having polycystic ovaries doesn’t automatically mean you have PCOS - it’s just one piece of the puzzle.
When viewed via transvaginal ultrasound, polycystic ovaries have distinct features that healthcare professionals are trained to recognize. This appearance is known as polycystic ovarian morphology (PCOM). To meet this diagnostic criterion, the ovaries usually show one of two things: 20 or more follicles per ovary or an ovarian volume of 10 cubic centimeters or more. These follicles often cluster around the ovary’s outer edge, creating a characteristic "string of pearls" look.
This enlargement happens because small, immature follicles accumulate. Unlike the large, solitary cysts seen in other conditions, these follicles remain underdeveloped. In a healthy ovary, one follicle matures each month to release an egg, while the others regress. In PCOS, hormonal imbalances disrupt this process, causing multiple follicles to develop but never fully mature.
Next, we’ll explore when and how ultrasounds are used to confirm these findings.
An ultrasound isn’t always necessary to diagnose PCOS. If you meet the other two criteria - elevated androgen levels and irregular ovulation - your doctor might not require one. However, ultrasounds are often used when the diagnosis isn’t straightforward or when additional confirmation is needed.
Timing matters when it comes to ultrasounds. For example, if you’re on hormonal birth control, your doctor may recommend stopping it for at least three months before the procedure. This pause allows your ovaries to return to their natural state, ensuring their appearance isn’t temporarily altered by the hormones.
Transvaginal ultrasounds provide the clearest and most detailed images of the ovaries. If you haven’t been sexually active, an abdominal ultrasound can be used instead, though it may not offer the same level of detail.
While ultrasounds are a helpful diagnostic tool, certain factors can influence how the results are interpreted.
Even with clear imaging, several factors can obscure PCOS features on an ultrasound. For instance, hormonal treatments like birth control or fertility medications, as well as recent pregnancy or breastfeeding, can temporarily alter ovarian appearance. Ethnic differences may also play a role - some women naturally have higher follicle counts, which could lead to overdiagnosis if not carefully evaluated.
Age is another important consideration. In teenagers and young adults, having multiple small follicles is relatively common and doesn’t always indicate PCOS. This is because their reproductive systems are still maturing, and these follicles may resolve over time.
Finally, the skill and experience of the technician and physician interpreting the ultrasound are crucial. Subtle differences between normal variations and PCOS-related changes can be tricky to spot. Inconsistent expertise across healthcare providers can sometimes lead to varying results, making it essential to seek experienced professionals for accurate diagnosis.
PCOS is diagnosed when at least two of the three criteria are met. Healthcare providers take a systematic approach, looking at how various symptoms and signs interact to create a clearer picture of reproductive health.
For instance, a diagnosis might be made if irregular ovulation and elevated androgen levels are present, even if polycystic ovaries don’t appear on an ultrasound. Alternatively, polycystic ovaries combined with irregular cycles could also indicate PCOS, even if there’s no obvious evidence of high androgen levels. These combinations reflect the variety of hormonal imbalances associated with PCOS.
This approach recognizes the diverse ways PCOS can manifest. Some individuals may have severe acne and excess facial or body hair while maintaining regular menstrual cycles. Others might experience irregular or absent periods without noticeable signs of elevated androgens.
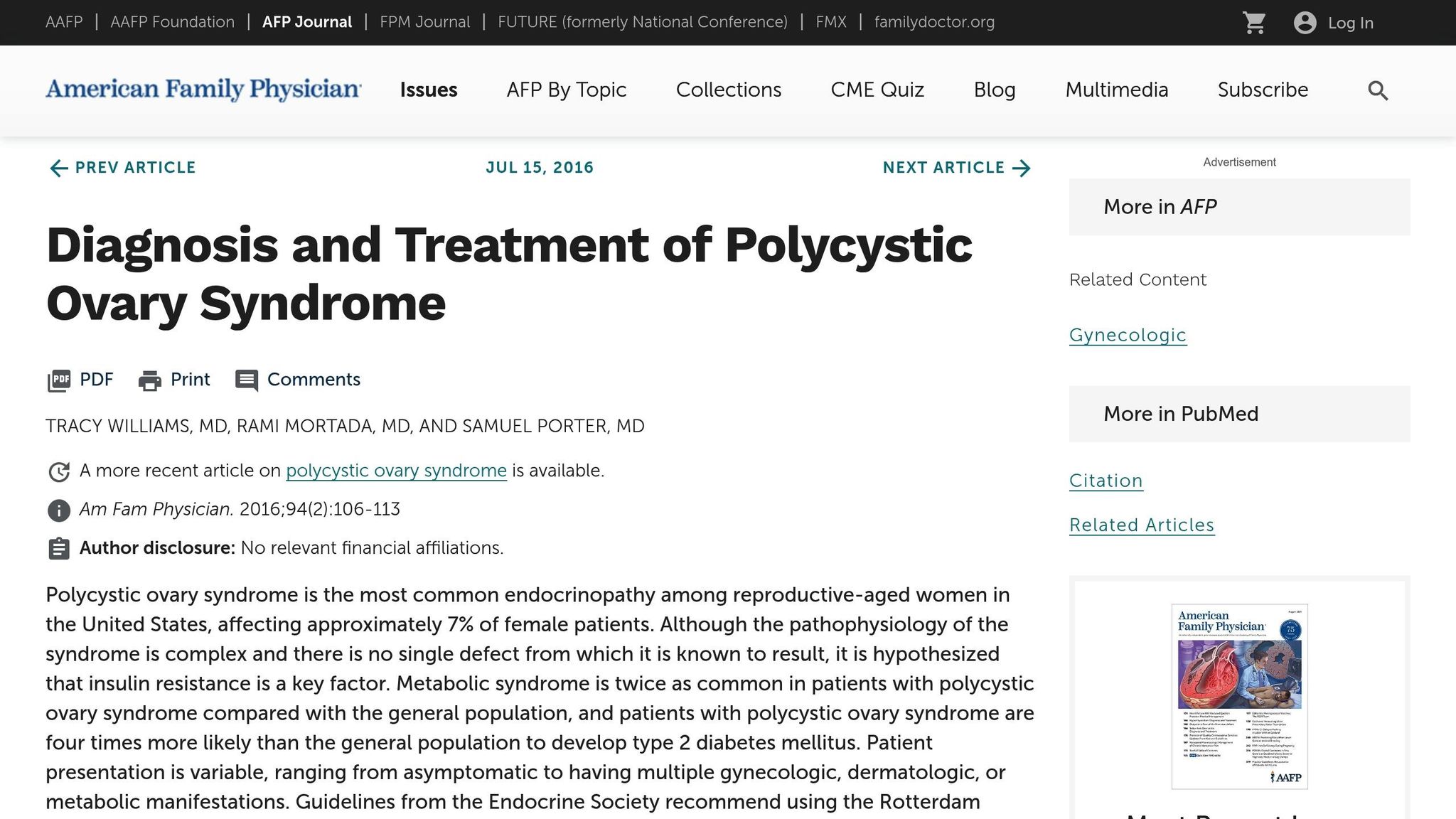
In 2003, the Rotterdam consensus introduced a widely accepted standard for diagnosing PCOS. The Rotterdam Criteria require the presence of any two out of three key markers: irregular ovulation, clinical or biochemical signs of increased androgen levels, and the presence of polycystic ovaries on ultrasound.
Before the adoption of these criteria, definitions of PCOS varied, leading to inconsistent diagnoses. Some older definitions required all three markers, while others focused primarily on irregular cycles and high androgen levels. By broadening the diagnostic scope, the Rotterdam Criteria acknowledged that PCOS can still be present even if one marker is less apparent. However, it also emphasizes ruling out other conditions that could mimic PCOS symptoms.
To better understand how these criteria work together, it helps to examine the clinical features, diagnostic methods, and considerations for each marker. The table below breaks down these details:
| Criterion | Clinical Features | Diagnostic Methods | Key Considerations |
|---|---|---|---|
| High Androgen Levels | Excess body or facial hair, severe acne, thinning scalp hair | Blood tests to measure testosterone and other androgens; clinical evaluation | Results may vary depending on menstrual cycle timing or the use of certain medications |
| Irregular Ovulation | Irregular periods (shorter than 21 days or longer than 35 days), absent cycles, unpredictable bleeding | Menstrual history, progesterone testing, ovulation predictor kits | Birth control can obscure natural patterns; stress and weight changes may temporarily impact cycles |
| Polycystic Ovaries | Often no external symptoms; identified via imaging | Ultrasound showing multiple small follicles or increased ovarian size | Factors like age, recent pregnancy, or hormonal treatments can influence ultrasound findings |
For example, borderline androgen levels combined with clear signs of irregular ovulation or polycystic ovaries on ultrasound strongly suggest PCOS. Similarly, visible signs of high androgens paired with irregular cycles can confirm the diagnosis, even without imaging.
This integrated approach offers a thorough framework for diagnosing PCOS. By understanding these criteria, you can have more informed discussions with your healthcare provider about your symptoms and diagnosis.
For more in-depth information on PCOS diagnosis and treatment, visit PCOSHelp.
Before diagnosing PCOS, healthcare providers carefully rule out other conditions that might share similar symptoms. This step is crucial to ensure you receive the right treatment.
Certain medical issues can mimic PCOS, making it necessary to conduct thorough evaluations. Below are some of the key conditions often mistaken for PCOS and the tests used to identify them.
To avoid misdiagnosis, healthcare providers assess several conditions with overlapping symptoms:
Diagnosing PCOS in teenagers presents unique challenges since irregular periods are common during the early years after menarche. The reproductive system is still maturing, making it harder to differentiate between normal development and PCOS.
For teens, healthcare providers usually wait at least two years after menarche before considering a PCOS diagnosis. During this time, they focus on managing symptoms like severe acne or excess hair growth while monitoring for patterns that suggest PCOS.
In contrast, adult women generally have more established menstrual cycles, streamlining the diagnostic process. However, factors like recent pregnancy, breastfeeding, or stress can still affect hormone levels and must be considered.
Family history also plays a larger role in diagnosing teenagers. Since PCOS often runs in families, a history of PCOS, diabetes, or metabolic conditions may prompt earlier evaluation and closer monitoring.
Symptoms of PCOS and their severity can vary widely among different ethnic groups, requiring tailored diagnostic approaches.
Recognizing these differences ensures that PCOS is diagnosed accurately and that treatment plans are tailored to address the unique risks and symptoms associated with each individual's background and genetics.
Diagnosing PCOS involves meeting at least two out of three criteria outlined by the Rotterdam Criteria: elevated androgen levels, irregular ovulation, and polycystic ovaries seen on an ultrasound. Here’s a closer look at these key markers:
It's also essential to rule out other conditions that might have similar symptoms. This is especially important for teenagers, as irregular periods are common in the first couple of years after their first period, and for women from various ethnic backgrounds, as symptoms can vary widely.
Getting the right diagnosis is a crucial first step in managing PCOS. PCOSHelp offers a wealth of resources to guide you through understanding your symptoms, exploring treatment options, and adopting self-care strategies. This information can help you work more effectively with your healthcare provider.
PCOS affects everyone differently, so there’s no one-size-fits-all approach. Reliable information empowers you to make informed decisions about your health and to advocate for the care that suits your unique needs.
Distinguishing PCOS from conditions like thyroid disorders or congenital adrenal hyperplasia (CAH) involves specific hormonal tests and a detailed evaluation by your healthcare provider. PCOS is generally diagnosed using three main criteria: hyperandrogenism (higher levels of male hormones), ovulatory dysfunction (irregular or absent menstrual cycles), and the presence of polycystic ovaries visible on an ultrasound.
In contrast, CAH is typically identified by elevated levels of 17-hydroxyprogesterone, which is not associated with PCOS. Thyroid disorders - such as hypothyroidism or hyperthyroidism - are diagnosed through thyroid function tests (TSH, T3, and T4) and often come with distinct symptoms like fatigue, changes in weight, or sensitivity to temperature, which differ from PCOS.
If you're noticing symptoms that seem to overlap, it's essential to consult your doctor for a thorough hormonal assessment to ensure you receive the correct diagnosis and treatment.
Managing symptoms of PCOS often begins with making lifestyle adjustments. Start by focusing on a well-rounded diet that includes low glycemic index foods, plenty of fiber, and sources of omega-3 fatty acids. Incorporating regular physical activity can help improve insulin sensitivity and support healthy weight management. Additionally, ensuring you get enough quality sleep and exploring ways to reduce stress can play a big role in maintaining overall well-being.
When it comes to medical treatments, your healthcare provider might suggest hormonal therapies, like combination birth control pills, to help balance hormones and lower androgen levels. Depending on your specific symptoms - whether it's irregular periods, acne, or insulin resistance - other medications might also be part of your treatment plan. Always work closely with your doctor to develop a plan that fits your individual needs.
Ethnicity and age play a key role in how Polycystic Ovary Syndrome (PCOS) symptoms show up and how the condition is diagnosed. For example, Non-Hispanic Black women may experience milder symptoms of PCOS compared to Hispanic and Non-Hispanic White women, with noticeable differences in traits like hyperandrogenism and metabolic health. Meanwhile, East Asian women often have a lower BMI and fewer visible signs of hyperandrogenism but face a higher risk of metabolic syndrome. These unique patterns can influence both the diagnosis and treatment strategies for PCOS.
Age also brings changes to PCOS symptoms. As women age, issues like hirsutism and acne often become less pronounced. At the same time, ovarian volume and follicle count naturally decrease, which can sometimes result in underdiagnosis or a shift in symptom presentation in older women. Recognizing these variations is crucial for ensuring accurate diagnosis and tailored management of PCOS across diverse groups in the U.S.