How Gut Dysbiosis Triggers Inflammation in PCOS
Explore how gut dysbiosis impacts inflammation in PCOS and discover effective dietary and lifestyle strategies for better management.
Explore how gut dysbiosis impacts inflammation in PCOS and discover effective dietary and lifestyle strategies for better management.
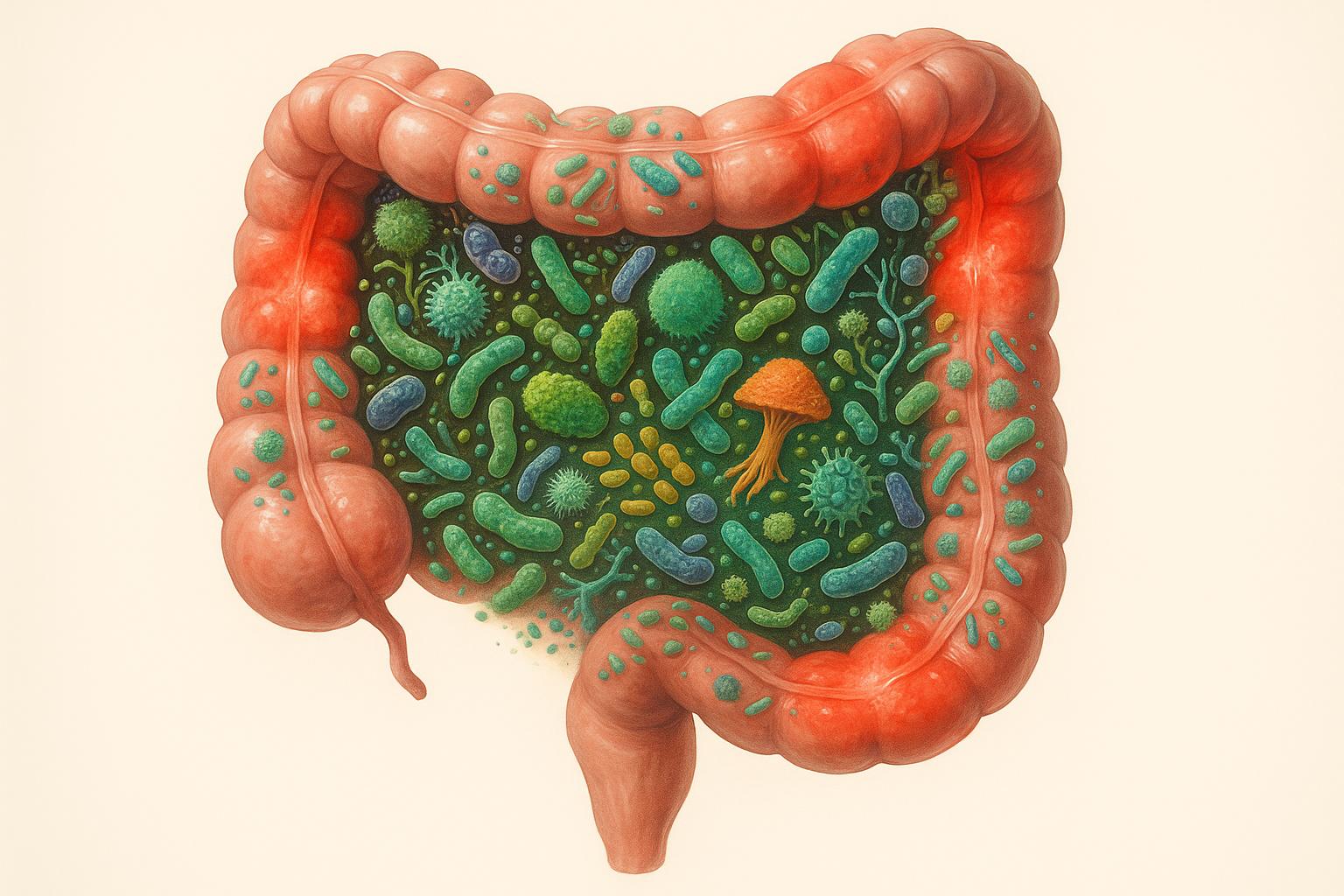
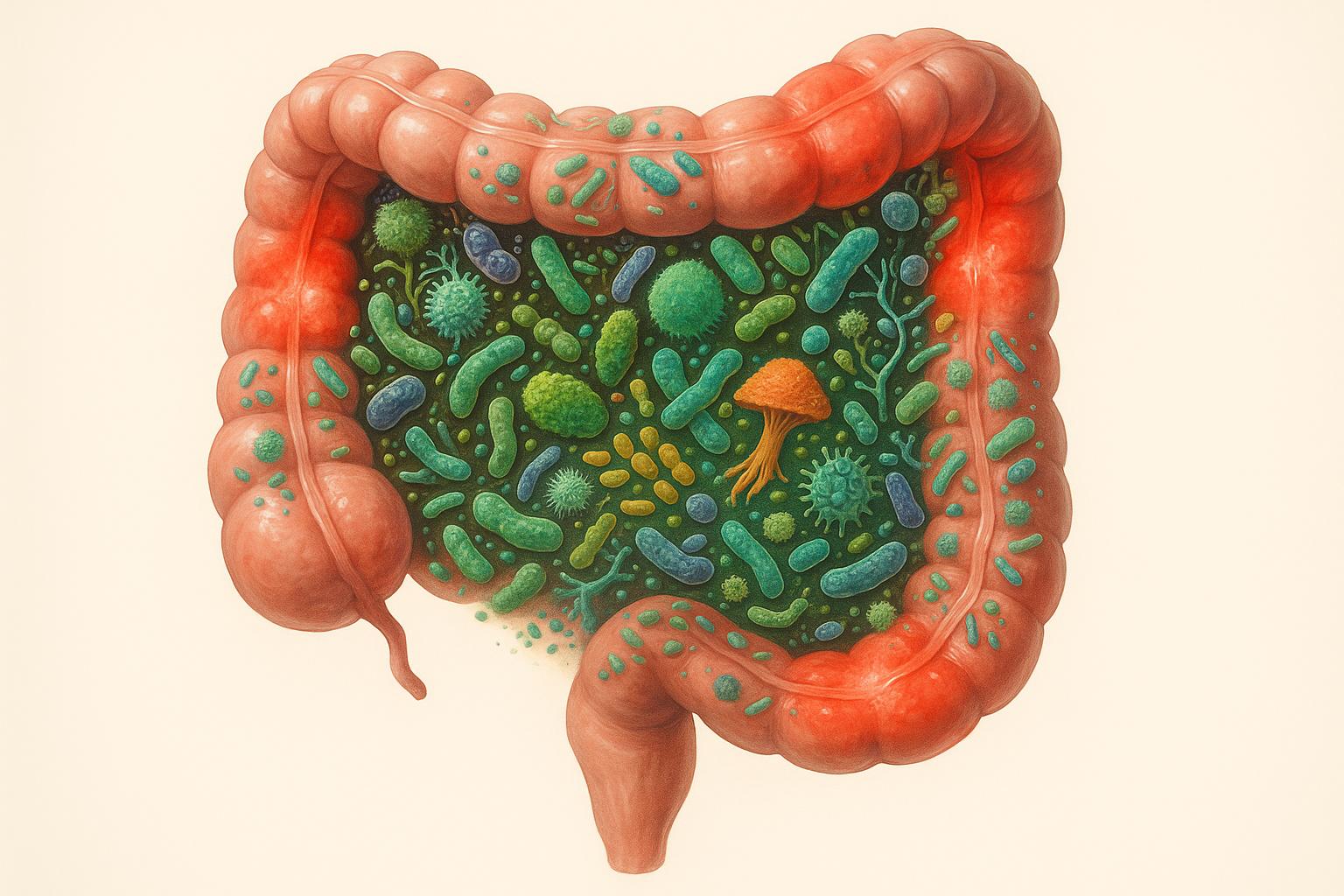
Gut health plays a major role in managing inflammation in PCOS. Women with PCOS often experience gut imbalances, or dysbiosis, which can worsen symptoms like insulin resistance, hormonal issues, and chronic inflammation. Here's what you need to know:
Emerging treatments like fecal microbiota transplants and postbiotics are also being explored to target gut imbalances in PCOS. Improving gut health could be key to managing inflammation and symptoms effectively.
Understanding how gut dysbiosis worsens PCOS symptoms requires a closer look at the biological mechanisms driving inflammation. The inflammation linked to PCOS often stems from three main factors: increased intestinal permeability (commonly called "leaky gut"), reduced production of short-chain fatty acids (SCFAs), and disruptions in bile acid processing.
Gut dysbiosis can weaken the intestinal lining, creating a "leaky gut" that allows harmful substances, like lipopolysaccharides (LPS), to escape into the bloodstream. These toxins, produced by certain bacteria, damage the tight junctions between cells in the gut lining. Once LPS enters the bloodstream, it triggers a strong immune response, leading to a surge in inflammatory cytokines such as TNF‐α, IL‐1, and IL‐6.
Research highlights the connection between LPS and inflammation. In one study, mice fed a high-fat diet for just four weeks developed obesity and insulin resistance, with LPS levels in their blood rising 2–3 times higher than those of control mice. Similarly, injecting LPS into healthy mice on a normal diet caused them to develop obesity and insulin resistance as well. For women with PCOS, who already experience elevated inflammatory cytokines, this LPS-driven inflammation can worsen insulin resistance and hormonal imbalances, intensifying symptoms.
Healthy gut bacteria play a crucial role in producing SCFAs like butyrate, acetate, and propionate when they break down dietary fiber. These SCFAs act as natural anti-inflammatory agents, helping to maintain the gut barrier and regulate immune responses. However, gut dysbiosis can significantly reduce SCFA production, leaving the gut more vulnerable to inflammation.
Studies suggest that increasing dietary fiber or supplementing with butyrate can help prevent obesity and improve insulin sensitivity. Without adequate SCFA levels, the body's defenses against both local and systemic inflammation weaken, further fueling the inflammatory processes linked to PCOS.
Gut bacteria are also essential for bile acid metabolism, which plays a key role in fat digestion and metabolic health. When dysbiosis occurs, this process becomes disrupted. Research by Qi et al. found that women with PCOS often show an overgrowth of Bacteroides vulgatus and a decrease in bile acid metabolites, along with reduced levels of the immune-regulating molecule IL-22.
This bacterial imbalance leads to excessive bile acid deconjugation and a reduction in critical metabolites like glycodeoxycholic acid and tauroursodeoxycholic acid. Lower levels of these metabolites reduce IL-22 secretion, weakening the gut's immune defenses and promoting inflammation. Additionally, impaired bile acid processing can disrupt the activation of metabolic receptors, such as the farnesoid X receptor (FXR) and Takeda G-protein-coupled receptor (TGR5), further contributing to metabolic issues and chronic inflammation in PCOS.
These interconnected pathways highlight the importance of addressing gut health as part of a comprehensive approach to managing PCOS symptoms. By targeting the gut, therapies may help reduce inflammation and improve overall metabolic balance.
Scientific studies have established a clear link between gut microbiota imbalances and inflammation in polycystic ovary syndrome (PCOS). These investigations reveal that the gut microbiome in individuals with PCOS undergoes specific changes that may directly contribute to the inflammatory processes associated with the condition.
Research consistently shows that women with PCOS experience notable shifts in their gut microbiome compared to those without the condition. For instance, a study conducted by Qi et al. demonstrated that fecal microbiota transplants from normal-weight women with PCOS into antibiotic-treated mice led to significant reproductive and metabolic changes. These included elevated testosterone and luteinizing hormone levels, which were not observed in mice receiving gut bacteria from healthy individuals.
Other studies highlight the presence of heightened inflammatory markers in women with PCOS. Elevated white blood cell counts, for example, have been found to correlate negatively with sex hormone-binding globulin (SHBG) levels and positively with testosterone levels and body mass index (BMI). This suggests a vicious cycle: gut dysbiosis fuels inflammation, which then exacerbates hormonal imbalances.
These findings pave the way for a closer examination of how bacterial profiles differ between women with PCOS and those without.
Delving deeper, research shows that women with PCOS exhibit lower gut microbiome diversity compared to healthy individuals. This includes a reduction in beneficial bacteria and an increase in harmful, pro-inflammatory species. A study by Pedro J. Torres and colleagues further explored this connection, finding a significant relationship between bacterial changes and hormone levels:
"These results suggest that hyperandrogenism may play a critical role in altering the gut microbiome in women with PCOS."
The study revealed that elevated testosterone levels and menstrual irregularities were closely tied to shifts in bacterial diversity, underscoring the role of hyperandrogenism in reshaping the gut microbiome.
| Bacterial Changes in PCOS | Effect | Impact on Inflammation |
|---|---|---|
| Increased Harmful Bacteria | Escherichia, Shigella, Bacteroides fragilis | Higher LPS production, increased systemic inflammation |
| Decreased Beneficial Bacteria | Lactobacilli, Bifidobacteria, Prevotellaceae | Reduced SCFA production, weakened gut barrier |
| Altered Metabolism Bacteria | Higher Bacteroides vulgatus, Lower Prevotella | Disrupted bile acid processing, increased BCAAs |
Studies from various countries consistently confirm these patterns. Research from China, for example, has shown that women with PCOS have significantly lower levels of beneficial bacteria like Lactobacilli and Bifidobacteria, as well as fewer Prevotellaceae. In contrast, harmful bacteria such as Escherichia and Shigella are more abundant, particularly in obese women with PCOS who tend to experience more severe gut microbiota imbalances.
These microbial imbalances amplify inflammation. Increased populations of gram-negative bacteria such as Bacteroides and Escherichia/Shigella produce more lipopolysaccharides (LPS), which can enter the bloodstream and trigger inflammatory responses. At the same time, reduced levels of beneficial bacteria lead to lower production of anti-inflammatory short-chain fatty acids and a compromised gut barrier.
These findings highlight the role of gut microbiota in driving inflammation in PCOS, laying the groundwork for therapeutic approaches that target gut health as part of broader PCOS management strategies. Consistent results across studies reinforce the potential for gut-focused interventions to help mitigate the condition's inflammatory and hormonal effects.
Addressing gut dysbiosis can play a key role in reducing inflammation linked to PCOS. Making thoughtful dietary choices, using targeted supplements, and adjusting lifestyle habits can help restore gut health, which in turn supports hormonal balance and lowers chronic inflammation.
What you eat directly affects your gut bacteria and overall inflammation levels, making diet a crucial part of managing PCOS.
Boost Fiber Intake
Fiber is essential for feeding beneficial gut bacteria and stabilizing blood sugar - important since insulin resistance impacts up to 75% of those with PCOS. Aim for 25 to 35 grams daily by including foods like broccoli, cauliflower, Brussels sprouts, leafy greens (such as arugula and red-leaf lettuce), beans, lentils, almonds, berries, sweet potatoes, winter squash, and pumpkin.
Add Anti-Inflammatory Foods
Incorporate foods known for their anti-inflammatory properties, like tomatoes, kale, spinach, almonds, walnuts, olive oil, blueberries, strawberries, and fatty fish such as salmon and sardines.
Cut Out Inflammatory Foods
Refined carbs are a major contributor to inflammation. Avoid white bread, pastries, sugary desserts, and processed foods hiding sugars like high-fructose corn syrup or dextrose. Beverages like soda and juice should also be limited.
Favor Plant-Based Proteins
Animal proteins can sometimes encourage harmful bacterial growth, so opt for plant-based proteins such as soy, legumes, and pea protein to support a healthier gut.
Choose Healthy Fats
Focus on omega-3-rich sources like fatty fish, nuts, seeds, avocados, and olive oil. It’s also wise to limit artificial sweeteners.
These dietary changes create a solid foundation for gut health, but supplementation can provide additional support.
Probiotics and prebiotics work together to restore gut balance and reduce inflammation. Probiotics help curb harmful bacteria, while prebiotics feed the beneficial ones. Research shows that taking probiotics for at least 12 weeks can improve metabolism, lower androgen levels, and reduce inflammation in PCOS.
Helpful Probiotic Strains for PCOS
Certain probiotic strains, such as Lactobacillus casei, L. acidophilus, L. rhamnosus, L. bulgaricus, Bifidobacterium breve, B. longum, and Streptococcus thermophiles, have been linked to lower insulin levels. Strains from Bifidobacterium and Lactobacillus families may also help reduce testosterone levels and symptoms like hirsutism.
Prebiotic Foods and Benefits
Prebiotics enhance beneficial bacteria and improve insulin sensitivity by increasing GLP-1 production. Include prebiotic-rich foods like tempeh, miso, yogurt, kimchi, and sauerkraut in your diet. Combining probiotics and prebiotics (synbiotics) may offer even greater benefits for insulin resistance, hormone balance, and lipid profiles.
Lifestyle changes are another critical piece of the puzzle for managing gut health and PCOS.
Lifestyle adjustments can significantly impact gut health and reduce PCOS-related inflammation.
Stay Active
Engaging in regular physical activity can improve insulin sensitivity and support hormonal balance. Aim for at least 150 minutes of moderate exercise or 75 minutes of vigorous activity per week.
Manage Weight
Losing even a modest amount of weight (5–10%) can help alleviate reproductive, metabolic, and psychological symptoms of PCOS. A balanced, calorie-conscious diet can assist with weight loss and symptom management.
Reduce Stress and Improve Sleep
Chronic stress and poor sleep are known to worsen inflammation. Practice stress management techniques and prioritize good sleep hygiene to maintain overall health.
Stick to Regular Meal Times
Consistent meal timing helps regulate blood sugar and supports healthy circadian rhythms, which can have a positive effect on energy levels and overall well-being.
Combining these lifestyle habits with dietary changes and the right supplements can make a big difference. As Amanda Stathos, M.S., R.D., L.D.N., explains:
"If you are diagnosed with polycystic ovary syndrome, it doesn't mean that you are destined to have poor health. There is a lot you can do to take charge, minimize symptoms and keep yourself healthy."
For more evidence-based tips on managing PCOS through diet, supplements, and lifestyle strategies, visit PCOSHelp.
Building on the connection between gut dysbiosis and PCOS-related inflammation, researchers are now exploring more tailored treatment options. These efforts go beyond traditional methods like probiotics and dietary changes, focusing instead on precision medicine that aligns with an individual's unique microbiome profile. This new direction offers a fresh perspective on managing PCOS inflammation.
Scientists are developing innovative therapies aimed at directly modifying gut bacteria to address inflammation linked to PCOS. One promising method is fecal microbiota transplantation (FMT). Unlike probiotics, which introduce specific bacterial strains, FMT involves transferring an entire healthy microbiome - including bacteria, viruses, fungi, and other microorganisms - into the patient’s gut.
Preliminary studies suggest that combining FMT with anti-inflammatory compounds like curcumin can reduce markers such as necrotic cells, insulin resistance, IL-6, and CRP levels. This has sparked interest in the potential of combination therapies using FMT and curcumin to restore microbial balance while reducing inflammation.
Another emerging approach involves postbiotics - bioactive compounds like short-chain fatty acids and bacteriocins produced during bacterial fermentation. These compounds have shown promise in improving gut barrier integrity, lowering systemic inflammation, and regulating glucose and lipid metabolism.
Additionally, CRISPR-Cas9 genome editing technology is being explored as a way to precisely modify gut microbial populations. This tool could allow scientists to promote beneficial bacteria while suppressing harmful ones, offering a highly targeted approach to managing gut health.
While these new treatments hold promise, personalized care is becoming increasingly important in managing PCOS. Traditional treatments often adopt a one-size-fits-all approach, but research suggests that tailoring interventions to an individual’s microbiome profile could yield better results. Advanced tools like metagenomic profiling now allow for detailed mapping of a person’s microbial community, helping identify imbalances and guide targeted interventions.
For example, a 12-week randomized controlled trial showed that supplementation with specific strains of Lactobacillus and Bifidobacterium significantly reduced body weight, BMI, fasting plasma glucose, and insulin resistance markers. Participants also saw improvements in lipid profiles, including lower triglycerides and VLDL cholesterol levels.
Comprehensive treatment plans that combine customized probiotics, personalized dietary recommendations, targeted exercise, and stress management strategies offer a holistic way to restore gut health and reduce inflammation. As research continues to uncover the intricate links between gut bacteria, inflammation, and PCOS symptoms, the potential for precision medicine to address the underlying causes of PCOS becomes increasingly clear.
The link between gut health and PCOS inflammation offers a promising path to better manage this condition, which affects up to five million women in the United States. When the gut microbiome is out of balance, it can trigger chronic inflammation through mechanisms like leaky gut, disrupted short-chain fatty acid production, and impaired bile acid processing. Understanding these connections provides a clear direction for more effective treatment strategies.
Research shows that women with PCOS have a gut microbiome that looks significantly different from those without the condition. They often have lower bacterial diversity and fewer beneficial microbes. This imbalance contributes to hallmarks of PCOS, such as hyperandrogenism, insulin resistance, and metabolic challenges, creating a cycle that worsens inflammation and symptoms over time.
Here’s the encouraging part: gut health can improve quickly, sometimes within just 24 hours, with small but impactful changes. Adjustments like eating more fiber, increasing the variety of plant-based foods, exercising regularly, and getting enough sleep can all enhance gut function and reduce inflammation. These simple steps address the underlying causes of PCOS-related inflammation, rather than merely masking the symptoms.
Emerging treatments, such as fecal microbiota transplantation, are also being studied as part of personalized care options. While these approaches hold potential, the foundation of PCOS management remains clear: a healthy gut is essential.
For the estimated 70% of women with PCOS who remain undiagnosed, and for those already navigating the condition, focusing on gut health can be transformative. By tackling gut dysbiosis, women can reduce inflammation, improve their symptoms, and take control of their overall well-being. Recognizing the deep connection between gut health and PCOS opens the door to meaningful, lasting improvements.
For more practical tips and personalized advice on managing PCOS through gut health, visit PCOSHelp.
An imbalanced gut microbiome, or gut dysbiosis, can make PCOS symptoms worse. It often leads to increased intestinal permeability - commonly called "leaky gut" - which allows harmful substances like endotoxins to enter the bloodstream. This process can spark chronic inflammation, further aggravating insulin resistance and raising androgen levels, both of which are central to PCOS.
Focusing on gut health through dietary adjustments, incorporating probiotics, and adopting anti-inflammatory approaches might help ease these effects. For more expert-backed strategies and practical advice, check out resources like PCOSHelp, which offers guidance on managing PCOS from a whole-body perspective.
Managing PCOS-related inflammation starts with taking care of your gut health. To support healthy digestion, include plenty of high-fiber foods in your diet, such as vegetables, legumes, and seeds. Adding fermented foods like yogurt, kimchi, or sauerkraut can help increase the beneficial bacteria in your gut. Whenever possible, choose whole grains over refined ones, and cut back on processed foods and added sugars, as these can throw off your gut's natural balance. Making small, steady adjustments to your eating habits can have a meaningful impact on your gut health and overall wellness.
Emerging approaches to address gut dysbiosis in PCOS include probiotics, prebiotics, and fecal microbiota transplantation (FMT). These methods focus on rebalancing gut bacteria, which could play a role in reducing inflammation and alleviating PCOS-related symptoms.
Probiotics and prebiotics help by nourishing and enhancing beneficial gut bacteria. On the other hand, FMT involves transferring healthy microbiota from a donor to help reset the gut's microbial environment. While these strategies show potential, further studies are needed to better understand their long-term safety and effectiveness. Be sure to discuss any new treatments with your healthcare provider before trying them.